Infectious Diseases Case of the Month |
||||||
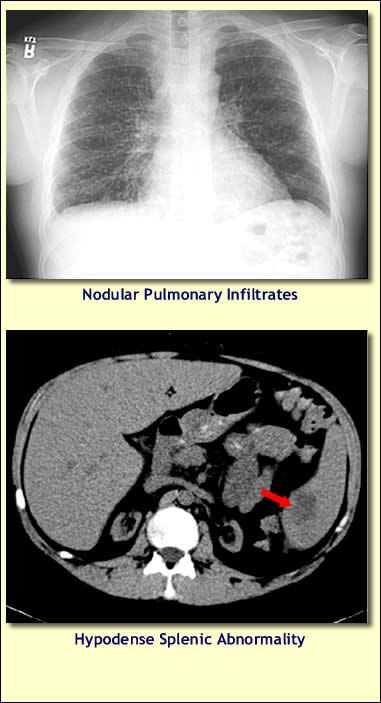 |
A 27 y.o. white male renal transplant patient was admitted to Munson Medical Center with severe dehydration after a two to three week history of nausea, vomiting, fever, and chills. He had first sought attention from his local physician. Symptoms, which also included a slight cough, did not respond to several days of levofloxacin. Eventually, imaging, including abdominal CT scan and CXR, was performed (see images at left). The CT scan showed a 3 cm subtle area of hypodensity in the spleen that the interpreting radiologist suggested was suspicious for a mass or an infectious process. The CXR showed numerous small non-calcified nodules distributed in a miliary pattern. Click here for larger CXR image. The patient was admitted to Munson Medical Center for further evaluation. On examination he appeared ill, had a temperature of 99.9, and was diaphoretic and hypotensive prior to receipt of IV fluids. He did not appear to be in respiratory distress and had no abnormal ascultatory pulmonary findings. Abdominal exam was benign. Initial labs included WBC 20.1, Hgb 8.8, creat 4.3. He had undergone renal transplantation 10 years earlier after renal failure secondary to membranous nephropathy. Anti-rejection therapy consisted of long term sirolimus, prednisone, and mycophenolate. He was married, had no known HIV or TB risk factors, and had not traveled outside of Michigan in recent months. Prior to his illness he was generally quite vigorous, and he worked as a landscaper. Family members had not been ill nor had their two pet dogs. The patient was placed on ampicillin/sulbactam and levofloxacin and in respiratory isolation. Empiric antifungal therapy was withheld because of concern for adverse drug-drug interactions (sirolimus). He underwent bronchoscopy on the evening of admission. At bronchoscopy the airways appeared to be normal. Specimens obtained (biopsies were not performed) were negative for significant pathogens including bacteria, fungi, pneumocystis jiroveci, and mycobacteria. Urinary legionella antigen was negative; urinary antigens for blastomyces and histoplasma were both weakly positive. CMV PCR was negative in blood. With receipt of fluids and anti-emetics the patient's prominent intestinal symptoms resolved and he felt well although he continued to have intermittent fevers. Nonetheless, the abnormal "miliary" pattern of pulmonary nodules persisted despite several days of broad spectrum antibiotic therapy. A diagnostic procedure was performed.
|
|||||
|
Answer and commentary will follow your submission. |
|||||