Infectious Diseases Case of the Month #7 |
|||
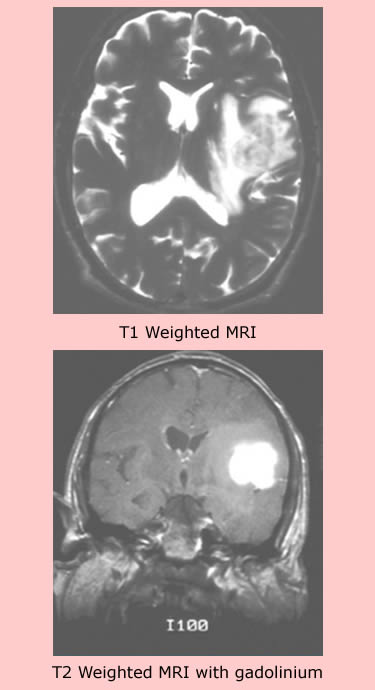 |
A 64 y.o. white male, a frequent traveler to the Philippines, presented to the emergency room with aphasia and right sided weakness and incoordination. A church minister, the patient had made many prior trips to the Philippines in connection with church missionary work. He had returned from his most recent two month trip to the Philippines two weeks previously. Nine months before his ER presentation he had been seen for fatigue and had 25% eosinophilia on peripheral smear. Examination of stools for O&P were negative 3 months prior to his acute neurologic illness. His Philippine church mission was on the island of Mindanao where he engaged in proselytizing and in various projects intended to improve the living circumstances of the local people. His family said that he had had numerous insect bites, consumed local foods, and had not had travel related immunizations. He had not taken anti-malarial prophylaxis.His past medical history was unremarkable and he took no medications on a regular basis (although he did take herbal and naturopathic remedies). He was married and had no history of high risk sexual behaviour. On examination he was afebrile with normal vital signs. He was noted to be aphasic and to have right upper extremity weakness and incoordination. Laboratory data included WBC 10.1 with 80% segs, 10% lymphs (no significant eosinophilia). Electrolytes, LFTs, and CXR were normal. An MRI scan was performed and showed a mass in the left fronto-parietal area (see images at left). Moderate mass effect was evident with compression of the lateral ventricle. In the emergency room he was evaluated by a neurosurgeon who was concerned about likely high grade glioma. The patient was placed on corticosteroids to reduce brain edema and underwent brain biopsy several days later. |
||
What organism is most likely to have caused this patient's illness? |
|||
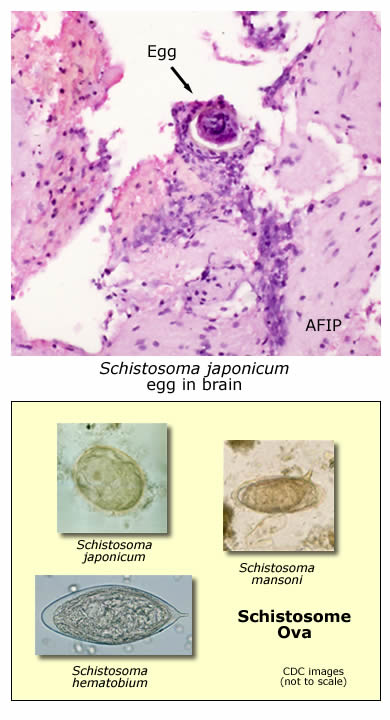 |
This patient had cerebral shistosomiasis caused by the eggs of schistosoma japonicum. A photomicrograph of the patient's brain biopsy is at left. Click here for a close up view of the schistosome egg. Schistosomiasis is a common infection with estimates of 200-300 million infected persons worldwide. Three species of schistosomes cause the majority of human illness. Schistosoma mansoni (Africa, South America, the Arabian Peninsula) and Schistoma japonicum (China, Indonesia, the Philippines) cause morbidity primarily related to the liver and portal tract. Schistosoma hematobium (Africa, the Middle East) causes disease primarily related to the bladder. Cerebral schistosomiasis, a form of neuroschistosomiasis, is an unusual complication of schistosomiasis. This complication occurs more commonly in patients infected with Schistosoma japonicum (compared to the other species) where it may occur in up to 2-4% of diagnosed cases. The pathogenesis of cerebral schistosomiasis is incompletely understood. Theories of pathogenesis include the oviposition of eggs by adult worms living ectopically in cerebral veins, the aberrant travel of eggs to the brain via the Batson’s plexus of vertebral veins, or the arterial embolization of eggs through porto-pulmonary anastamoses or via previously developed pulmonary arteriovenous shunts. Why japonicum ova are more likely to cause cerebral schistosomiasis is not known. It has been suggested that the greater fecundity of the gravid adult japonicum worm and/or the smaller, rounder shape of the japonicum ova and their smaller or absent lateral spines might be more apt to allow distant embolization. Eggs of the three different schistosome species are pictured at lower left. This patient had a "tumorous" form of cerebral schistosomiasis (disease can also occur in a more disseminated "diffuse" form). Diagnosis was confirmed by pathologists at the AFIP and by serologies. The patient was treated with praziquantel and high dose corticosteroids (for inflammation and edema). As praziquantel is not ovicidal, corticosteroid therapy was necessarily prolonged (to allow time for the eggs to spontaneously die and inflammation subside). His neurologic recovery was eventually essentially complete. Had this patient been evaluated in an endemic area, brain biopsy may not have been necessary and empiric therapy with praziquantel could have been employed much as it commonly is done for neurocysticercosis, another parasitic central nervous system disease. This case highlights how "small" the world has become with the ease and frequency of international travel.
Ref: Pittella JEH, Neuroschistosomiasis. Brain Pathology, 7:649-662, 1997.
|
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||