Infectious Diseases Case of the Month #6 |
|||
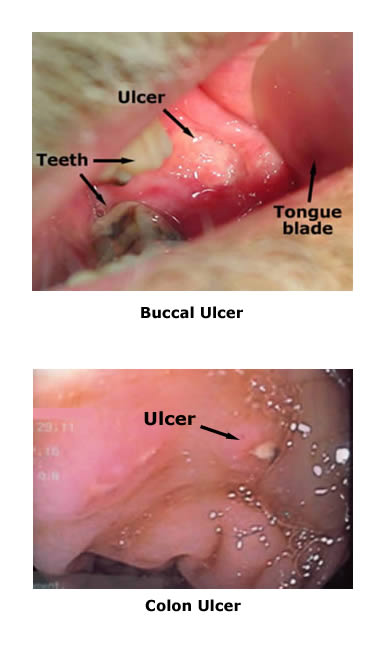 |
A 60 y.o. white male with rheumatoid arthritis was admitted to the hospital for syncope. This was the patient's third hospitalization within the previous two months related to an undiagnosed systemic illness. This illness began approximately three months prior to the current hospitalization and was originally characterized by pulmonary symptoms (cough and shortness of breath) treated with a course of prednisone. The illness later came to be more prominently characterized by high irregular fevers, wt loss, malaise, and intermittent prostration. The two previous hospitalizations were for a prior syncopal spell and a left lower extremity deep venous thrombosis respectively. He had suffered from rheumatoid arthritis for the previous ten to fifteen years. Previously treated with methotrexate, he had experienced significant relief of his symptoms since therapy with Humira was initiated five or six months prior to his current hospitalization. He lived in rural northern Michigan on family property where there was an old barn frequented by pigeons. He had not traveled beyond the Midwest recently but had been to Indianapolis to visit a son a month or so before he became ill. In his previous evaluations he had undergone an extensive work up for infectious diseases, malignancy, and hypercoagulability without conclusive results. Studies had included blood cultures, serologies and CT Scans (chest CT had shown areas of interstitial and nodular infiltrates). A bone marrow biopsy done for thrombocytopenia had shown granulomas but no organisms were seen on AFB or fungal stains. Admitting labs included WBC 5.2, Hgb 12.9 (L), Plts 145 (L), AST 35, ALT 74 (H). On examination he appeared ill and had high fever but had no focal findings except for buccal ulcers (see upper left). While undergoing evaluation he experienced diarrhea and had an abrupt fall in hemoglobin with evidence of intestinal bleeding. He underwent upper and lower gastrointestinal endoscopy and was found to have ulcers throughout his intestinal tract including stomach, small bowel and colon. A representative colon ulcer is pictured at lower left. Multiple biopsies were taken from ulcers in the upper and lower gastrointestinal tract, and he had a repeat bone marrow biopsy. |
||
What micro-organism is most likely to have caused this patient's illness? |
|||
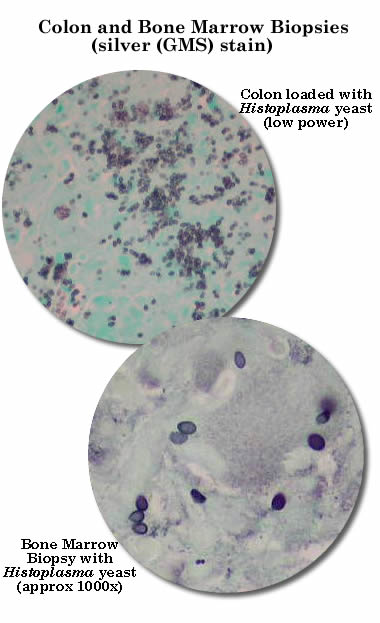 |
This patient had disseminated histoplasmosis where the drug Humira may have played a predisposing role. Histoplasmosis is a disease caused by the dimorphic fungus Histoplasma capsulatum. This fungus is found throughout the world but is more prevalent in certain regions of North and Central America, particularly the Mississippi and Ohio River valleys in the United States. Histoplasmosis can manifest in a variety of ways but most commonly with symptoms related to disease of the respiratory tract. Disseminated histoplasmosis, as in the case described, tends to occur in persons with immunocompromising conditions. It can present as an FUO and can be a rapidly progressive, even fatal disease particularly in those severely immunosuppressed. Diffuse involvement of the gastrointestinal tract is described. In the case described this individual had widely disseminated disease. Biopsies (see photomicrographs at left) of his bone marrow and throughout his intestinal tract were positive histologically and microbiologically. In addition he had evidence of pulmonary and hepatosplenic involvement. The patient has been started on itraconazole with initial clinical improvement and resolution of fevers. This case is of particular interest for two reasons. The first is the potential role played by Humira (adalimumab), a human tumor necrosis factor (TNF) antibody. Use of such agents has provided significant relief to persons with illnesses such as rheumatoid arthritis and crohn's disease. Unfortunately, these agents appear also to predispose to the development of serious infectious diseases particularly tuberculosis. The manufacturer's product literature explicitly states a need to be careful using this drug in persons living in areas where tuberculosis and/or histoplasmosis are endemic. Also of interest is the use of the histoplasma urinary antigen for diagnosis of histoplasmosis. This can be a highly sensitive test for histoplasmosis particularly in cases of disseminated disease where the test has up to 90% sensitivity. Though not mentioned in the case history, this test was done in the case described; a highly positive result prior to the more invasive tests helped lead to the patient's diagnosis.
Ref:Wheat, L.J., Kauffman, C.A., Histoplasmosis, Inf Dis Clins NA, 17:1, pgs 1-19, March 2003. |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||