Infectious Diseases Case of the Month Case #40 |
|||
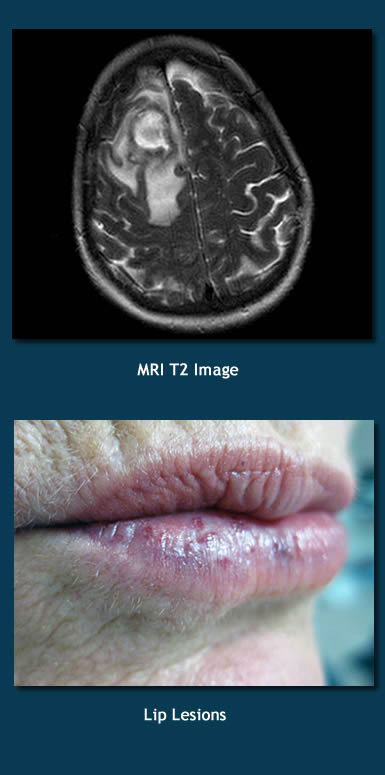 |
A 61 year old white female was admitted to the hospital for a brain abscess discovered after she had presented with confusion. Previously healthy, she had been experiencing headaches for a week or more prior to her emergency room presentation and also had had sweats and perhaps low grade fevers. Her confusion had manifested more acutely and was perhaps best exemplified by her getting lost when driving her car in what should have been very familiar locales. Imaging at the time of her emergency room presentation was notable for the finding of a 3 x 3 x 3 cm enhancing right frontal lobe lesion with surrounding edema (see MRI at left). Findings were thought most consistent with a brain abscess, and the patient was begun on vancomycin, metronidazole, ceftriaxone, and dexamethasone. At the time of her emergency room evaluation she was afebrile and had otherwise normal vital signs. She appeared slightly confused and had mild weakness of her left sided extremites. She had subtle lesions of her lips that were chronic (see image lower left) and a grade 1/6 systolic murmur. There were no peripheral stigmata suggestive of of infective endocarditis (splinter hemorrhages, etc). The patient had history of head trauma from a fall two years earlier. Neuroimaging (MRI) at that time had not shown significant abnormality. She had history of mitral valve prolapse. She did not have history of significant dental or chronic sinus problems although she did have history of multiple severe nosebleeds as a child. She did not have history of intravenous drug use but did consume alcohol in moderation. She had undergone acupuncture treatment three days before her hospitalization in attempt at treating her headache. She was self employed providing body piercings and tattoos. Her family history was notable for the fact that her father had died of a cerebral hemorrhage when he was 26 years old. On the second hospital day she underwent stealth stereotactic biopsy of the lesion. Seven cc of yellowish brownish fluid was initially aspirated. Three days later she underwent a second neurosurgical procedure to further drain the abscess and had a drain placed. Preliminary culture data indicated the growth of a gram positive organism. Which of the following most likely underlay this patient's development of a brain abscess? |
||
What was the likely predisposing factor in the development of this abscess? |
|||
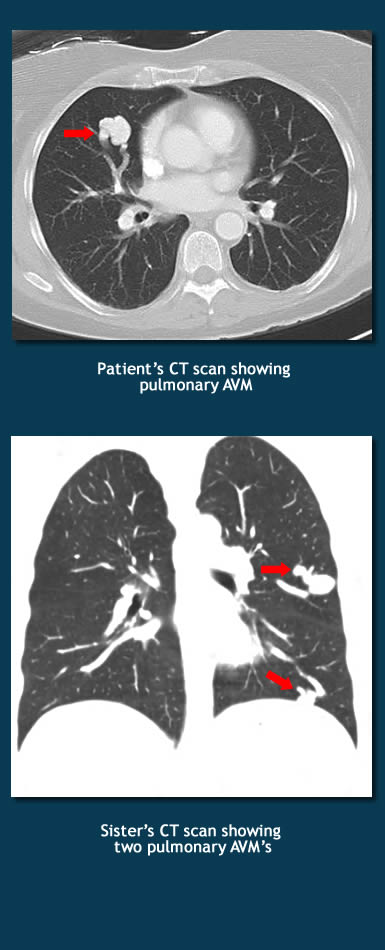 |
The patient’s brain abscess was caused by Streptococcus anginosus. The underlying predisposing factor was the presence of a pulmonary arteriovenous malformation (AVM) which in turn derived from the patient’s previously undiagnosed hereditary hemorrhagic telangectasia (HHT) syndrome. Hereditary hemorrhagic telangectasia syndrome is a disorder of the development of the vasculature characterized by the presence of multiple arteriovenous malformations (AVM’s) that lack intervening capillaries resulting in direct communication between arteries and veins. Smaller AVM’s are called telangectases. Telangectases are most evident on the lips, tongue, face, and fingers and nasal, buccal, and gastrointestinal mucosa. They are apt to bleed because of their thin walls, tortuous paths, and lack of vessel wall contractile elements. AVM’s proper (larger telangectases) are commonly defined as arteriovenous communications of a few millimeters or larger in diameter. AVM’s occur most commonly in the liver, lung, and brain. In contrast to the bleeding from telangectases, complications from AVM’s relate to shunting of blood (increased cardiac output plus when AVM's occur in the lung, arterial desaturation). In pulmonary AVM’s there can also be right to left shunting of venous emboli (clots or bacteria). Most individuals with pulmonary AVM's have HHT. Brain AVM’s due to HHT are typically congenital whereas AVM’s of lung and liver may develop over time. Often undiagnosed, hereditary hemorrhagic telangectasia is a genetic disorder estimated to have a prevalence in North America of 1/10,000 (likely an underestimate). Mutations in at least five genes are thought to result in HHT. Diagnosis depends on the presence of multiple AVM’s/telangectases in characteristic locations. Consensus criteria have been developed for diagnosis. An early manifestation of disease is typically severe childhood epistaxis, but the syndrome displays age related penetrance with increased symptoms developing over a lifetime. The brain abscess described in the preceding vignette presumably arose as a consequence of right to left shunting of bacteria across the large pulmonary AVM (image upper left or click here for a larger image). The patient underwent coil embolization of the AVM to obliterate it. Investigation of the patient’s family identified several members who also likely had HHT. One sister also had lip telangectases, had history of severe epistaxis and GI bleeding, and had two pulmonary AVM’s discovered upon investigation (see image lower left). In retrospect, it would seem likely that the patient’s father’s death due to cerebral hemorrhage at age 26 was due to rupture of a cerebral AVM related to the presence of HHT. Streptococcus anginosus group bacteria are a common cause of pyogenic abscesses including those involving the brain (see Case #35). The other potential predisposing factors in the preceding vignette can also lead to infection under certain circumstances. Dental infection, in particular, can predispose to brain abscess but was not the likely cause here. Ref: McDonald, J., et al, Hereditary hemorrhagic telangectasia: an overview of diagnosis, management, and pathogenesis, Genetics in Medicine 13 (7): 607-616, 2011 |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||