Infectious Diseases Case of the Month #15 |
|||
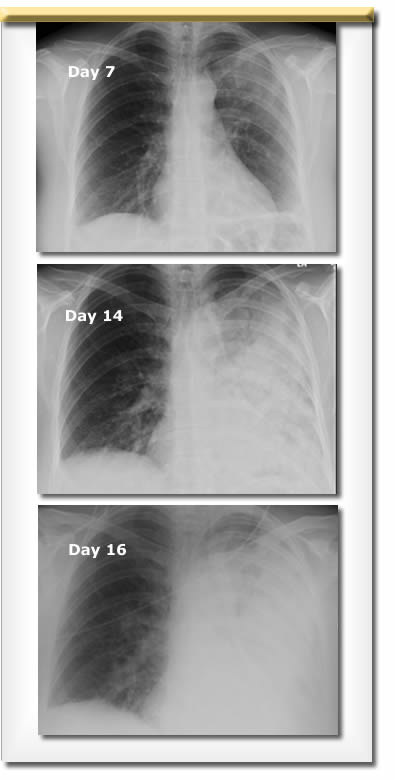 |
A thirty-six year old white female was admitted to the hospital for progressive subacute pneumonia. Previously healthy her first indication of illness had come two weeks previously when she developed left sided chest pain followed by the development of fevers and malaise. She was seen by her primary care physician three days after the onset of symptoms who prescribed levofloxacin 250 mg daily for likely pneumonia. A week into her illness she presented to the emergency room with ongoing symptoms including cough that was sometimes productive. An CXR suggested pneumonia (see image at top left). She was advised to increase her levofloxacin to 750 mg daily. On day 14 of her illness (day 11 of levofloxacin) she was referred for admission to the hospital by her primary care physician as she had shown no clinical improvement and her CXR had significantly worsened (see middle image at left). She appeared moderately ill and had diminished breath sounds and crackles in her left lung. There were no skin lesions. A CT scan of her chest (not pictured) showed dense, nearly complete, consolidation of her left lung without apparent abscess or pleural effusion. At the time of admission her temperature was 98.7, BP 115/69, pulse 117. Admission labs included WBC 21.6, hgb 13, plts 502. Oxygen saturation was 98% on 3L O2 by nasal cannulum.The patient was married, the mother of two young children, and worked as a medical transcriptionist. She had no HIV risks nor other known immunocompromising conditions. Other family members had not been ill nor had their two dogs. She and her family lived in rural northern Michigan (near Traverse City) and spent many weekends at a family lake property in Michigan's Upper Peninsula (map). The lake cabin was attached to a boathouse that was frequented by bats, and the family had noted an extensive amount of bat droppings in the boathouse. She had been very busy at the end of the school year taking her children on field trips to the shore of Lake Michigan and Mackinac Island but had otherwise not traveled out of the local area. On admission to the hospital she was begun on IV piperacillin-tazobactam and vancomycin. Despite this she became progressively more ill with high fevers, shortness of breath, and the appearance of peri-hilar infiltrates in her right lung as well (see lower image at left). Blood cultures and sputum cultures were without significant growth, and urinary legionella and pneumococcal antigens were negative. On the fourth hospital day she underwent bronchoscopy. Evidence of bronchitis was not found but there were copious thin greenish secretions. Specimens were obtained by protected brush and bronchoalveolar lavage and submitted to the lab for evaluation. |
||
What organism caused this patient's progressive pneumonia? |
|||
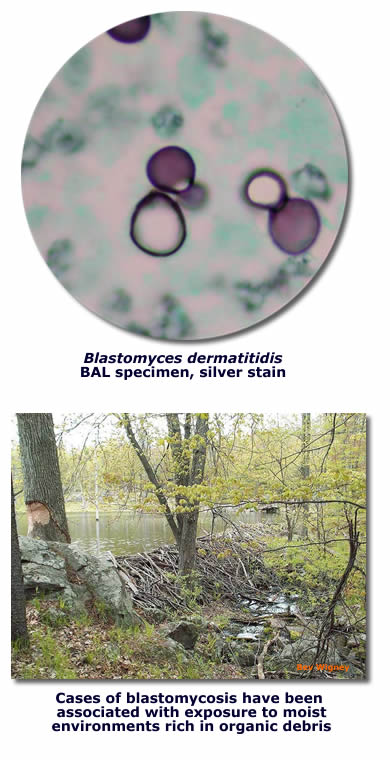 |
This patient had severe pneumonia secondary to Blastomyces dermatitidis. Immediately after the patient's bronchoscopy she was started on IV itraconazole because of concern that she may have fungal infection. Examination of BAL specimens showed broad based budding yeasts consistent with Blastomyces dermatitidis (see image, upper left) . Because of the life threatening nature of the patient's pneumonia she was switched to liposomal amphotericin B. She required a prolonged period of mechanical ventilatory support before she began to show improvement. After improvement was evident she was switched back to itraconazole for an extended course of therapy. In the course of her evaluation Blastomyces urinary antigen was positive and fungal cultures also ultimately grew B. dermatitidis. Urine Histoplasma antigen was negative. Blastomyces dermatitidis causes a variety of clinical syndromes. In most cases it causes pneumonia manifest radiographically as alveolar or mass-like infiltrates. The next most common radiographic appearance of pneumonia is that of reticulo- The epidemiology and ecology of blastomycosis have been difficult to define because of the lack of sensitive skin tests or serology and the difficulty of isolating B dermatitidis from nature. Therefore case reports of disease in humans and dogs have formed the basis for what is known of its epidemiology. In the United States most cases have been reported from Mississippi, Arkansas, Kentucky, Tennessee, and Wisconsin. It is believed that the organism grows in the soil of moist wooded areas rich in organic debris. In a rare instance where B. dermatitidis was isolated in nature associated with an outbreak of human disease, it was isolated from the site of a beaver dam along the Eagle River in Wisconsin. Perhaps that site appeared similar to that pictured at lower left. Persons infected with blastomycosis are more apt to be males pursuing outdoor occupational or recreational pursuits. The other organisms featured in the choices in the preceding vignette (see original format) also are capable of causing severe pneumonia. Legionella longbeachae would not be identified by legionella urinary antigen testing but would likely have been responsive to levofloxacin. Histoplasma capsulatum was a prime suspect in this case because of its association with bat droppings, but pneumonia manifesting as a densely consolidated unilateral process on CXR would not be typical. Methicillin Resistant Staphyloccus aureus would likely have caused more acute disease than was observed in this case and would have likely shown some response to vancomycin. Franciscella tularensis can cause severe pneumonia but would likely have responded to levofloxacin. Ref: Bradsher, R.W., et al, Blastomycosis, Infect Dis Clin N Am 17 (2003) 21-40. |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||